
Falls are common. Each year one in every three people aged over 65 will fall. Around one in ten falls lead to serious injury. Most of us have a friend or relative who has experienced an injury from a fall and know what a life-changing event it can be.
The most common serious injuries are fractures and brain injuries. Falls can also result in a loss of confidence, which can lead to restriction of activity and a lower quality of life. Many older people never regain their pre-fall level of function and might even struggle to keep living by themselves.
The consequences of falls cost Australia a staggering $4.3 billion every year. The good news is 20-30% of falls among older Australians can be prevented.
Why do we fall in older age?
Falls happen when there is a mismatch between our physical abilities and the immediate demands of the environment or activity being undertaken.
Falls become more common as we get older because as we age, there is a natural decline in muscle strength, balance and vision, all of which are important for helping us stay upright.
The risk of falls is increased by certain medical conditions (such as Parkinson’s disease, dementia and stroke) and certain medications (such as sleeping tablets).
But this doesn’t mean falls are inevitable.
Exercise makes the most difference
Exercise that aims to improve balance and leg strength is the most effective in preventing falls.

This means exercise that is carried out while standing (not while seated), with the feet positioned close together or while standing on one leg (if safe to do so), while performing controlled movement of the upper body (leaning and reaching movements, for example).
Balance training combined with strength training for the major muscle groups is most effective.
These exercises need to be tailored to individual abilities. Middle-aged people with good physical function will benefit from harder exercises (such as functional training at a gym or boot camp incorporating squats and step-ups).
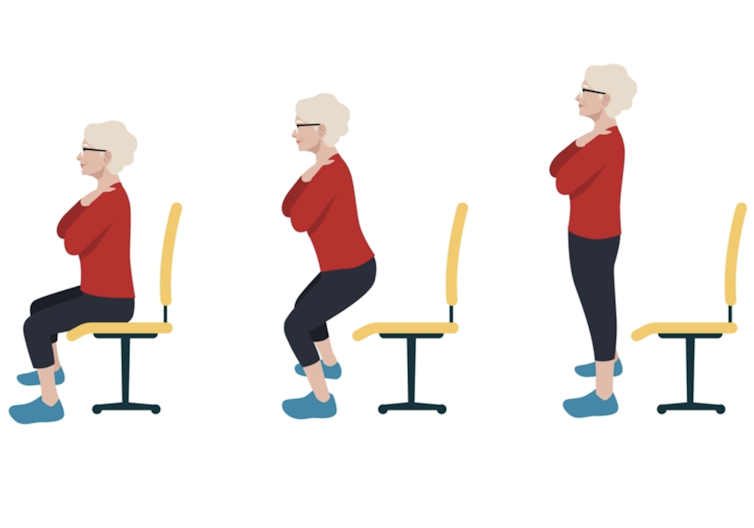
Effective exercises for people with impaired physical function or frailty will follow the same principles but should be modified for safety and effectiveness. These include everyday activities such as standing up from a seated position without using arms for support, walking up and down stairs, walking in one line, stepping over obstacles or balancing on one leg.
Read more: The search to extend lifespan is gaining ground, but can we truly reverse the biology of ageing?
For lasting impacts, it’s important this type of exercise is done often. The World Health Organization recommends incorporating these exercises two to three times a week as part of the 150-300 minutes a week of moderate activity recommended for improving health.
Not everyone enjoys exercising, which means some people struggle to prioritise it. It’s very important to know nobody is ever “too old” to start exercising, and benefits are gained at any age. But don’t hold off to start exercising either – the earlier we start to build our strength and balance, the better off we will be in our older years.
Starting small and building up the amount and intensity of activity, and choosing something enjoyable, are the best ways to start. If you can’t reach a high dose of exercise initially, any amount is better than nothing.
If you like exercising in a group, consider finding a local program and invite a friend along for added support and social connection. Your state government or local council should have their classes listed online.
If you’re not sure where to start, the best thing to do is to seek professional help to select exercises that suit your abilities and health conditions. Talk to your GP, local physio or exercise physiologist.
What else can we do to prevent falls?
In addition to exercise to improve balance and strength, other actions that can reduce the risk of falls include talking to your doctor or pharmacist to review your medications, seeing a podiatrist if you have painful feet, and maximising the safety of your home environment by installing adequate lighting and grab rails, and ensuring walkways are free from clutter and liquid spills.

Falls are not inevitable as we age. We need investment in strategies to help older Australians stay active and independent, and avoid falls. Despite knowing what works to avoid them, we have no national policy or strategy to implement and fund fall prevention programs. Doing so would not only help older Australians, but the budget bottom-line too.
Anne Tiedemann receives funding from the National Health and Medical Research Council.
Cathie Sherrington receives funding from the National Health and Medical Research Institute.
Kim Delbaere receives funding from the National Health and Medical Research Council. Kim Delbaere is the President of the Australian and New Zealand Falls Prevention Society.
* This article was originally published at The Conversation

0 Comments