Fibromyalgia causes debilitating pain. Healthy gut bacteria soothed symptoms in a small trial.
Imagine waking up every day after a full night’s sleep feeling completely fatigued. Every muscle hurts. But you don’t have a fever or an infection. After years of diagnosis, doctors can’t tell you why the pain keeps growing. Painkillers offer little help. Eventually, you can no longer walk—and still, there’s no explanation.
That’s the story of Rina Green who has fibromyalgia, a mysterious condition that affects roughly four percent of the population, mostly women. Its symptoms are varied. Most people experience chronic debilitating pain, fatigue, sleep disruptions, and brain fog. Over time, nearly half develop depression. The pain can be so severe that, like Green, they can no longer walk or take part in daily activities.
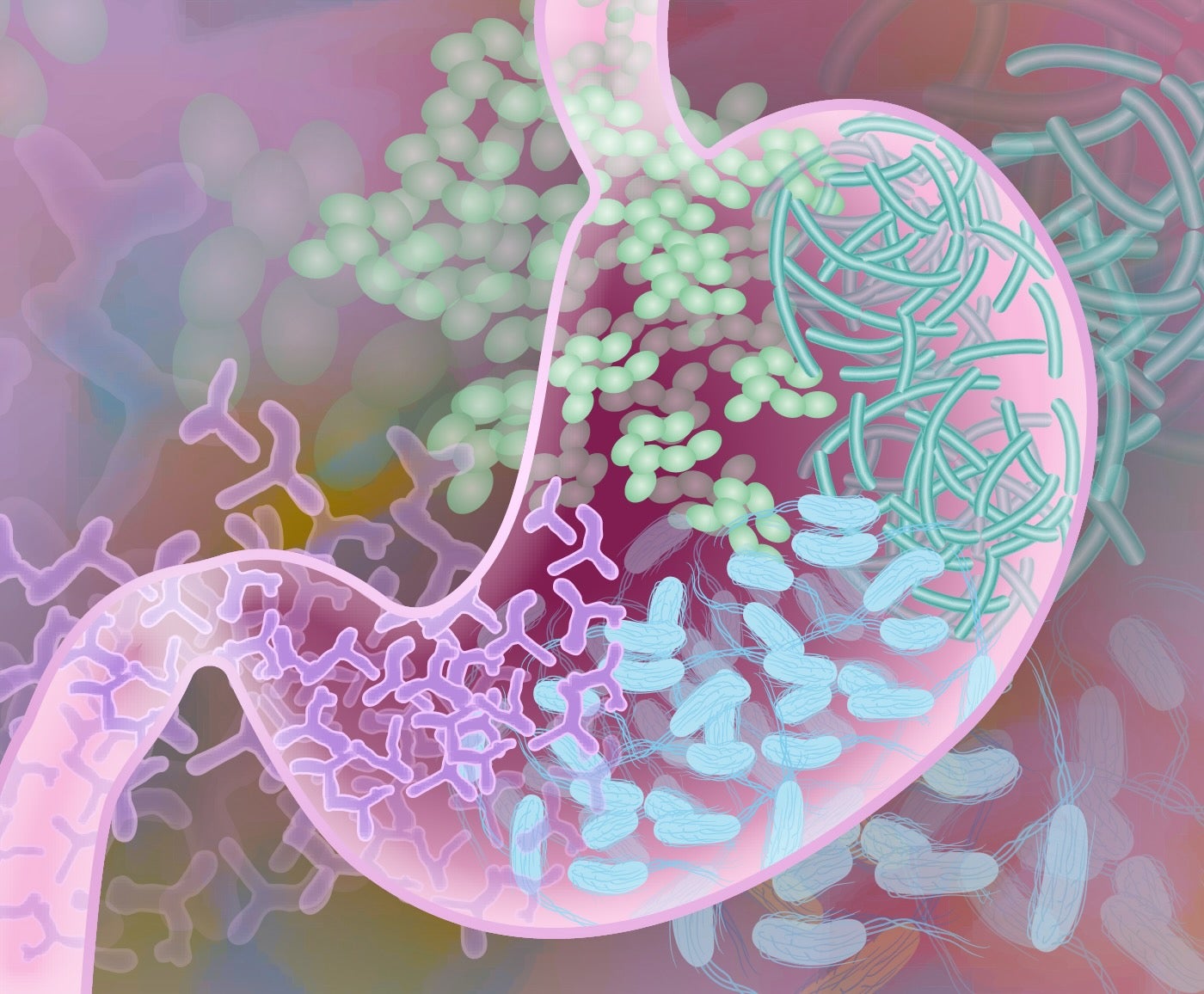
Unlike a paper cut or scraped knee, fibromyalgia isn’t linked to obvious damage to tissues or organs. The condition was once believed to be just in patients’ heads. More recent studies, however, have found signs of dysfunctional nerve connections and inflammation throughout the nervous system in people with the disease. Their immune systems are out of whack, and so are their gut microbiomes—the collections of bacteria living in our digestive systems.
A new study in Neuron now suggests that the gut microbiome may be key to treating the disease. In a small clinical trial, 14 women with severe fibromyalgia took pills containing healthy, living gut bacteria from donors. Within a month, nearly all reported decreased pain. Green, now 38 years old, was able to leave her wheelchair and take short walks.
The results are the latest to highlight a connection between gut bacteria and the brain. Tinkering with this connection—through probiotics, for example—may offer a way to tackle chronic pain without directly accessing the brain using opioids or other painkillers.
A Microbe Universe
We’re more microbe than human. A recent estimate suggests we carry three times more bacterial cells than human ones. They’re not just along for the ride. Over the past decade, scientists have linked various health outcomes to the mixture of microbes in the gut.
Some are tied to the brain. Called the gut-brain axis, scientists have shown that gut bugs can influence anxiety, depression, and memory depending on which chemicals they release. These might diffuse into the blood or zap nerves and send signals to the brain.
Older studies found people with depression or other brain disorders have altered gut microbiomes. Because microbes live synergistically with us, they pump out different chemicals—some of which impact the brain, depending on their type and abundance. Some researchers are hunting down these chemicals as they relate to mental health or antibiotic-resistant gut problems. Others are taking a simpler approach: Replacing “dangerous” bacteria with helpful bugs from healthy donors through a procedure called fecal microbiota transplant.
The strategy has been used to treat irritable bowel syndrome, antibiotic-resistant infections, and pain related to chemotherapy. More trials are testing if it can boost cancer immunotherapies.
In 2019, study author Amir Minerbi, director of the Pain Medicine Institute at the Rambam Health Campus in Israel, and colleagues found that the gut microbiome shifted in women with fibromyalgia. Comparing the microbiomes of 77 women with the condition to 79 without, they used AI to highlight signatures related to the disorder.
This led the team to wonder: Do altered microbiomes trigger chronic pain?
Mediator of Pain
In the new study, the team first transplanted gut bacteria from women with or without fibromyalgia into mice. The animals had their microbiomes wiped out, allowing the new arrivals to settle.
In just a month, those receiving microbes from donors with fibromyalgia began experiencing similar symptoms. They were more sensitive to pain from pressure, cold, and heat. The mice also seemed to feel pain without stimulation. But their health was mostly intact otherwise.
The picture changed at four months. The animals began showing signs of depression similar to their donors. Their nerve signals also changed over time, pumping out excessive neuroactive chemicals that amp up data transmission—which could contribute to increased sensitivity to pain—and their immune systems shifted towards a more inflammatory response.
These symptoms were treatable with a two-step program. First, the team dosed the mice with antibiotics to wipe out “bad” gut bugs. Next, they transplanted microbes from healthy donors into their guts. The treated mice were perkier, with nearly normal sensitivity to pain.
Encouraged by the results, the team recruited 14 roughly middle-aged women with severe fibromyalgia. Despite taking at least two painkillers and undergoing lifestyle tutoring, all participants still struggled with excruciating pain and daily fatigue.
After purging gut bacteria with antibiotics, each participant received five microbiome transplants from healthy donors, once every two weeks, in the form of a pill.
The new bugs took hold inside their guts roughly a month after the first treatment. One week after the last treatment, 12 people reported less pain associated with cold or heat. They felt less anxious or depressed, and most were finally able to get a good night’s sleep.
“These findings are really impressive,” Andreas Goebel at the University of Liverpool, who was not involved in the work, told Nature.
Next Steps
Though promising, the study has its limits.
For one, it’s open-labeled, meaning both researchers and patients knew they were getting the treatment. That means placebo effects could be a factor in why they felt less pain. The study also only included women and female mice. The reason for this, explained the team, is that fibromyalgia predominately affects women. But the results pave the way for the approach to be studied in a larger, more diverse group of people.
The team is planning a randomized controlled clinical trial—the gold standard—in roughly 80 people. They’re also hoping to pin down specific bacterial species and environmental factors involved in pain, such as stress, infections, and other diseases. And they’re investigating several molecules and signaling patterns discovered in the study that differ in people with fibromyalgia.
For now, we can say “altered gut microbiota has a role in fibromyalgia pain, highlighting it as a promising target for therapeutic interventions,” wrote the team.
The post Patients Say Healthy Gut Bacteria Relieved Their Chronic Pain in a Puzzling Disease appeared first on SingularityHub.
* This article was originally published at Singularity Hub

0 Comments